Managing chronic conditions is a major process in every correctional setting. The chronic care visit is an ideal time for…
Read More
Nursing Practice
EIGHT WAYS TO IMPROVE CLINICAL JUDGMENT
I am often asked how correctional nurses can improve their critical thinking/clinical judgment. In response, here are some ways to…
Read More
Being Mindful of Biases in Clinical Evaluations
I love the simple, yet powerful words of Dr. Seuss, but nurses might steer themselves in the wrong direction if…
Read More
Correctional Nurse Professional Practice: Understanding the Ethical Considerations in Correctional Nursing
In the healthcare realm, the role of a correctional nurse stands at the intersection of healthcare and criminal justice systems….
Read More
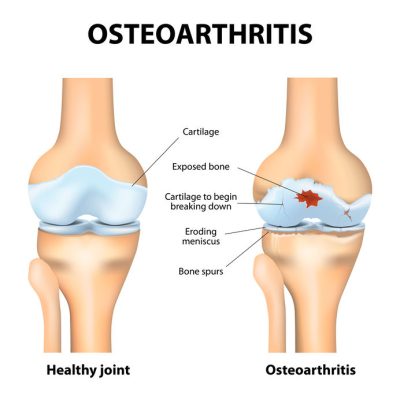
Correctional Nurse Clinical Update: Osteoarthritis
Osteoarthritis and Rheumatoid Arthritis are both debilitating diseases that affect millions of individuals in the United States. In the correctional environment,…
Read More
Correctional Nurse Practice: The Unique Roles of LPN/LVNs and RNs in Corrections
Correctional nursing presents unique challenges, including working within a confined environment; managing diverse health issues that may have been neglected…
Read More